Bengaluru, 21st February, 2025: In a remarkable case highlighting the importance of early detection and cutting-edge surgical techniques, a two-day-old baby underwent minimally invasive hernia repair surgery for left-sided Congenital Diaphragmatic Hernia (CDH). A condition that occurs only in 1 out of every 5000 delivered babies, CDH is a rare condition where a defect in the diaphragm allows abdominal organs to move into the chest cavity, impairing lung and heart development. 80% of CDH cases occur on the left side, 10% on the right side and the rest 10% being bilateral.
In this case, the condition was recognized antenatally, that is while the mother was still pregnant with the baby, during a routine anomaly scan at 22 weeks. Advanced pre-natal imaging technology revealed characteristic signs of CDH in the baby such as bowel or intestinal loops present in the chest cavity, displacing the lung and heart tissue. But the initial signs were hopeful as the baby had already developed the lungs with there being no high pulmonary blood pressure or heart and chromosomal anomalies. This encouraged the doctors to expect a positive result when the baby was delivered.
Also Read: Eat right for your heart to beat right
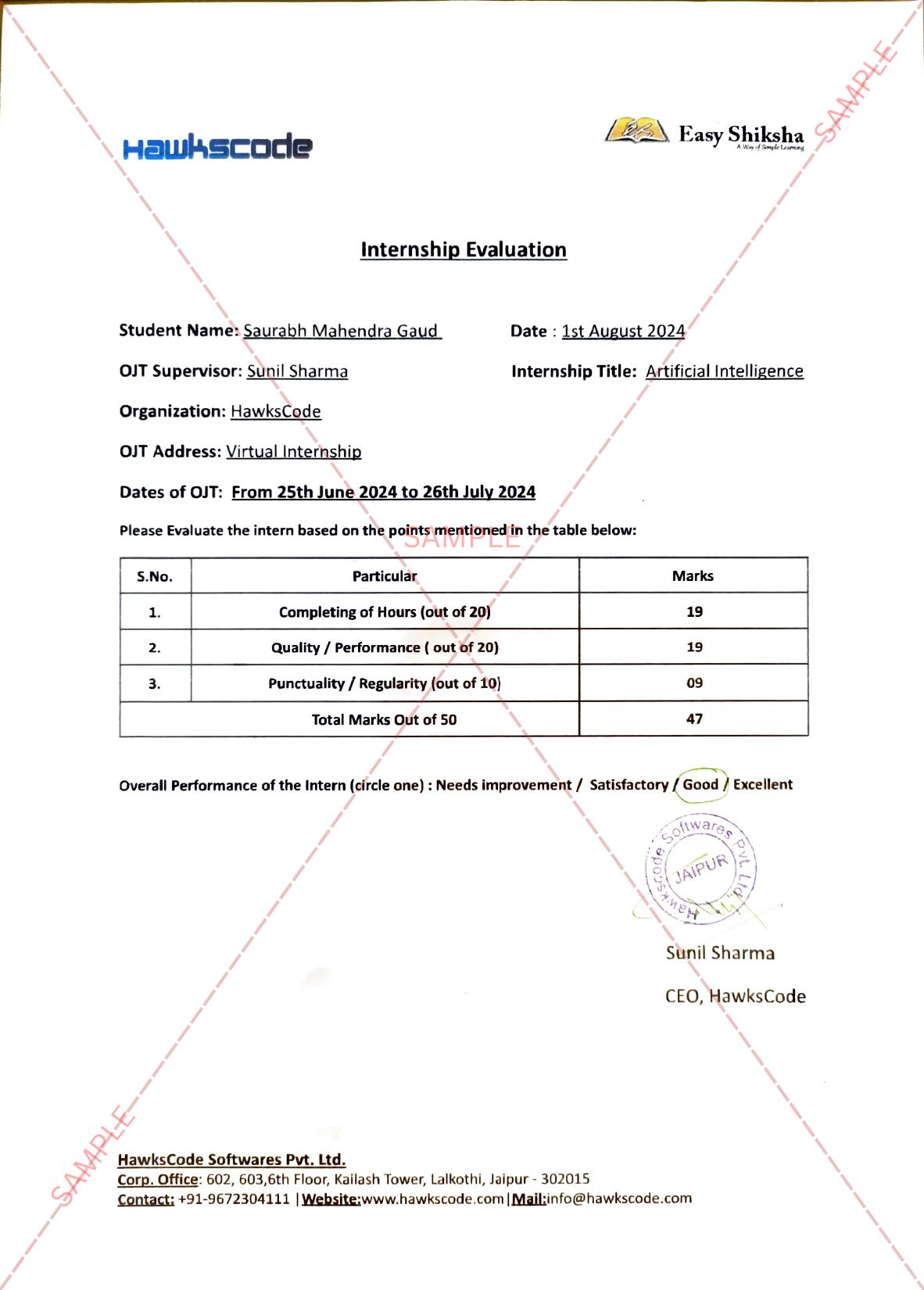
The mother underwent a c-section and delivered a son weighing 3 kgs on 3rd January 2025. X-rays done post-delivery confirmed the diagnosis. Echocardiograms were used to determine there was no pulmonary hypertension. The baby demonstrated well-developed lungs, normal pressure gradients and stable cardiovascular function. Additionally, the defect in the diaphragm was small, with only intestines as contents and the absence of major structural anomalies. Spontaneous breathing of the baby was good, it did not require ventilatory support after birth. These factors made the baby a suitable candidate and the team at Aster Whitefield Hospital decided to go for a minimally invasive thoracoscopic surgery to treat his CDH.
The surgery was performed 48 hours after the child’s birth to allow stabilisation. Pediatric surgeries, especially ones that are done on new-born babies, are very complex as well as tricky due to the delicacy of the condition. The operating room is always kept warm to prevent hypothermia. For this procedure, very small 3 mm incisions were made to insert the thoracoscope (a camera attached to a telescope) and other surgical instruments. After detecting the anomaly, the intestines were reduced to the abdominal cavity and the diaphragmatic defect was meticulously sutured using non-absorbable stitches. The neonatal, paediatric and anaesthesiology team performed the entire surgery under continuous monitoring to ensure stability.
“The surgery went smoothly without any complications. The anesthesia team was highly attentive, carefully monitoring the baby’s oxygen levels, blood pressure and temperature during the procedure. The surgery was made more manageable due to the coordinated effort among all teams involved, including neonatologists, anesthesiologists, and pediatric surgeons”, said Dr. Manjiri Somashekhar, Lead & Senior Consultant – Paediatric Surgery, Aster Women & Children Hospital, Bengaluru. “As a result, no immediate complications were encountered, and the baby’s condition was stable throughout”, she added.
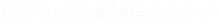
Dr. Lathiesh Kumar, Lead Neonatology, Consultant – Paediatrics and Neonatology, Aster Women & Children Hospital, Bengaluru mentioned, “Minimally Invasive Thoracoscopic surgery offers numerous advantages, including minimal trauma, reduced pain, faster recovery and shorter hospital stays. But not every child suffering from CDH is eligible for such a surgery, due to the many complications involved. This case was only the second instance of thoracoscopic repair out of six CDH cases managed by the team in the past two years.” Online Courses with Certification
Online Courses with Certification
Post-surgery, the baby required only 24 hours of ventilatory support, a stark contrast to the extended care often needed in traditional open surgeries. The chest tube used during the procedure to drain out any excess air, fluid, or blood collected during the surgery was removed within 24 hours and the baby was able to transition to tube feeding shortly after. The baby was discharged in 5 days post operation. The parents underwent multiple counselling sessions to completely understand the situation and be prepared.
While there is no one particular reason behind the development of such a condition in the child, potential causes include folic acid deficiency, maternal smoking, alcohol consumption, certain medications or pre-existing health conditions like diabetes or hypothyroidism. The key message for parents is that early detection and proper counseling are essential. If a congenital anomaly like CDH is identified, parents should seek advice from experienced surgeons and neonatologists to understand the treatment options available. This case underscores the importance of early detection, proper antenatal counseling, and immediate post-birth stabilization. This story stands as a beacon of hope for families facing similar challenges, demonstrating that with timely intervention and expert care, a bright future is possible.
Platforms like EasyShiksha.com offer valuable courses that can help you gain the necessary skills.